During the COVID-19 pandemic, CDC encouraged healthcare facilities and providers to implement telehealth strategies to manage chronic patient conditions as well as other care needs while practicing social distancing. In March, HHS Secretary Alex Azar announced a “historic expansion of telehealth access to combat COVID-19” with CMS offering expanded Medicare coverage for telehealth visits. The incorporation of telehealth into the norm of patient care is expected to continue to rise post-pandemic, as the technology is touted to increase value, affordability and access to resources.
Derek Rockwell, Chief Information Security Officer & VP of Product Engineering will be speaking during a complimentary fireside chat with critical healthcare stakeholders | July 28, 12 pm ET | Register now for Defend Against MedTech Cyber BreachZipnosis is one of numerous companies that offer a platform to facilitate virtual care. In a Q&A with MedTech Intelligence, company COO Catherine Murphy discusses several aspects of virtual care: It’s adoption, the benefits for patients and providers, improving the user experience and patient safety.
MTI: What impact is the rapid adoption of telehealth visits having on the healthcare system?
Catherine Murphy: In light of the ongoing pandemic, the healthcare industry, which has historically been slow to change, is being forced into fast innovation and adoption of virtual care. Health systems, providers and patients are not only seeing that virtual care is possible across new clinical specialties—but that it [also] works. For example, in just a few months we saw one of our health system partners go from completing just a handful of behavioral health visits virtually to over 2,000. Patients will no longer accept a “one-size-fits-all” argument for all care being in-person care. Virtual care has proven it’s worth and value—there’s no going back to the status quo.
MTI: What are the unique benefits of using telehealth as a means of interacting with patients?
Murphy: Every patient’s care needs are unique, and virtual care provides flexibility in how both patients and providers engage with one another.
Care is a continuum, and virtual care gives us the power to offer flexible, quality and convenient care to patients. Virtual care enables health systems to provide patients with in-person care when it’s needed, and treat them online when it’s not. And with virtual care, all modes of care have their place—it’s the overall experience for patients that matters most.
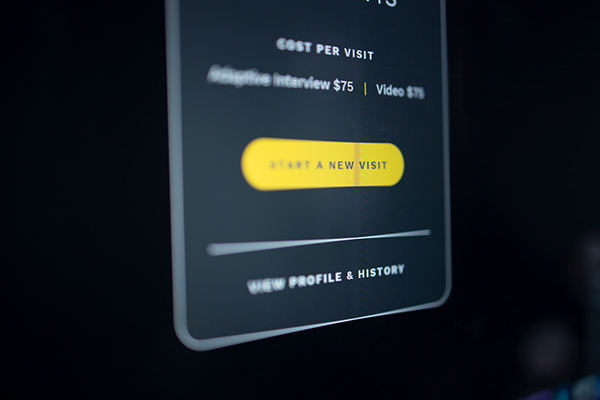
On [the Zipnosis] platform, providers are also able to move between modes of care at the click of a button. If a provider has a question about a patient’s initial asynchronous intelligent interview responses, they can ‘step-up’ a visit to video, phone or chat in order to learn more. Virtual care is no longer limited to a simple video visit, or a single phone call. Virtual care truly allows providers to connect with patients in a more personalized way.
Virtual care also helps improve provider work time. Especially in moments, like we experienced during this pandemic, when patient visit volumes significantly increase. When COVID-19 first hit the United States, we were able to quickly train and activate additional providers for our health system. While some telemedicine companies struggled with 20-hour wait times, our health system partners were able to maintain an under [a] 10-minute wait time, and a 4:33 minute average clinical work time over all four modes of care.
MTI: What considerations should designers of this type of technology take into account?
Murphy: Virtual care is often applied in treating low acuity conditions. However, virtual care can be activated in any clinical specialty. It’s critical designers of this type of technology think outside the box of what virtual care is now, instead looking towards what it can be in the future.
Designers should continue to innovate with the end user in mind—both patient and provider. Historically, good user experience has been rare in healthcare, but if virtual care is going to truly innovate how healthcare is provided, user experience can’t be an afterthought, especially for providers who are burdened by hours of visit and other documentation in their EMR. Designers of virtual care technology can continue the momentum of adoption going forward by reimagining new ways to simplify healthcare, while also taking the burden off health systems to build these tools themselves.
MTI: Are there patient safety concerns (thinking in terms of misdiagnosis)? If so, how is this technology mitigating any risks?
Murphy: With any patient care, there are always patient safety concerns. In fact, studies have found that with in-person care, provider adherence to clinical guidelines care varies depending on the time of day the decision is made.
However, with asynchronous virtual care in particular, we’ve found providers are actually more likely to provide clinically appropriate care. This is because we are able to build clinical decision logic right into our platform. And it’s proven to work. In a study conducted in 2019, we found Zipnosis clinical algorithms helped achieve nearly 90% adherence to clinical guidelines.

MTI: Would you like to add anything else about working with patients in a virtual care capacity?
Murphy: As COVID-19 visits and the need to order testing increased across the country, our team saw an increased need to help providers order and manage testing remotely. With that in mind, we developed ZipTicket for COVID-19. This essentially allows providers to order COVID-19 testing (both diagnostic and antibody testing), within the context of a virtual visit. ZipTicket COVID-19 also supports testing in a lab, a drive through facility, or at-home testing. For in-person testing, the patient simply selects a testing location, the lab is notified, and the patient arrives with their ZipTicket ‘boarding pass’ to receive testing. With at-home testing, patients simply enter their address and a test kit is sent directly to their home.
This is functionality we originally offered for treating strep, but have quickly expanded it to meet health systems needs to address more testing demands, like COVID. We believe this is a powerful tool for connecting virtual care with in-person care in the future.







