MTI: What is the medical community doing to educate patients about this type of therapy versus drug treatment?
Burton: There are 250,000 primary care physicians in the country. I think they’re all increasingly aware that the use of chronic opioid is challenging and in some cases dangerous. There’s a large addiction and dependence problem in the United States; there were more deaths from opioid overdoses in 2014 than there were from car accidents. A lot of physicians are out in the trenches, but it’s hard to deliver a relevant and understandable message to a quarter of a million physicians. To get the message out about alternative therapies is also challenging. One of the difficult things about pain is that there are many conservative treatments for it. In most patients that we see for neuromodulation therapies, they’ve tried and exhausted these therapies (over-the-counter medications, massage, exercise programs, aquatic therapy and chiropractic care). When you get beyond that, people get into different physical medicine approaches and physical therapy, and other non-opioid medications. Then they try surgical corrective therapies.
Getting the message out about options for chronic pain is complicated. I think we’re getting there. We have different professional societies (the North American Neuromodulation Society, The American Academy of Pain Medicine, The American Society of Anesthesiology) that try to educate medical colleagues about available options.
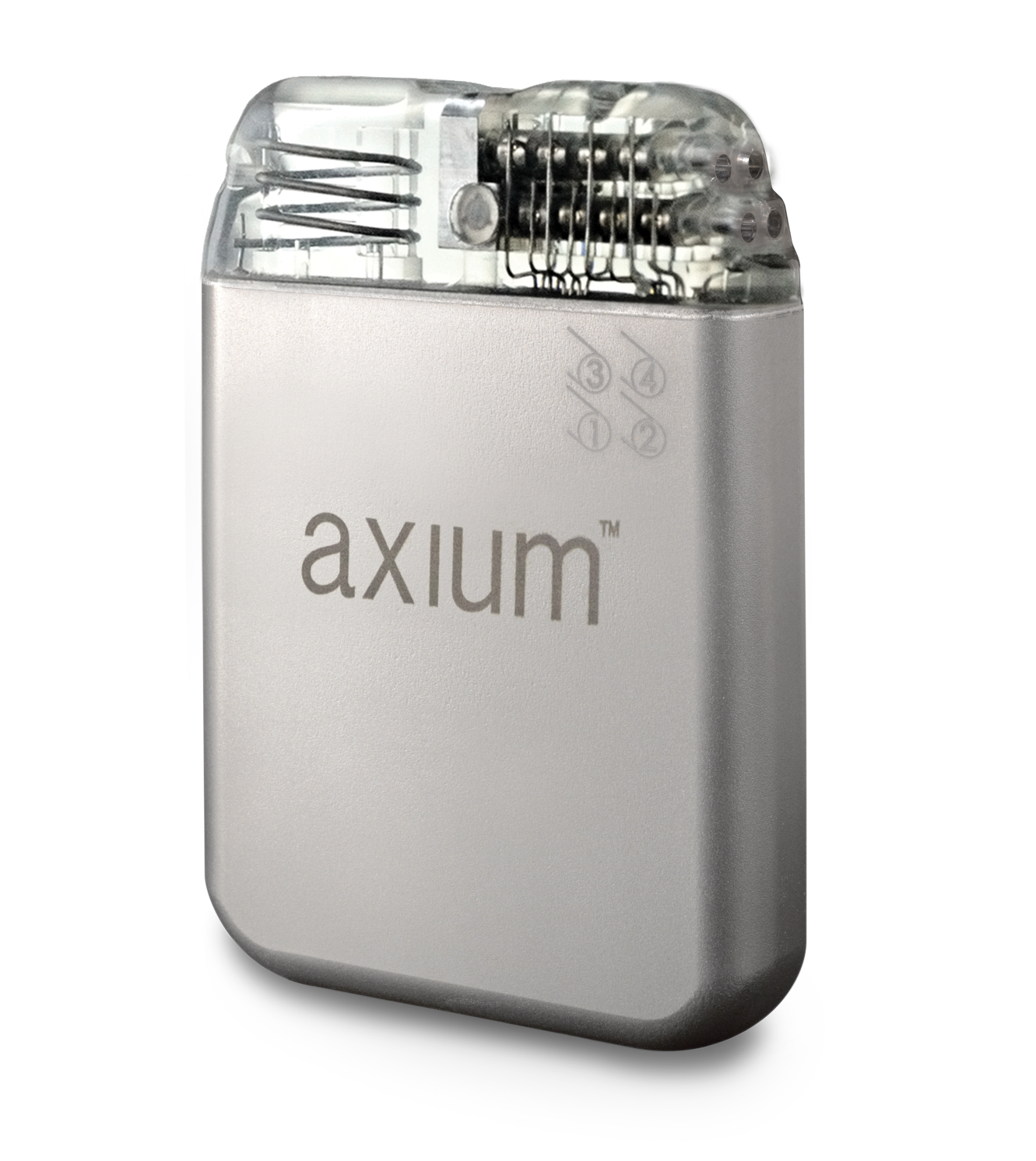
I think neuromodulation technologies have made significant advances in the past two to three years. The old technologies used to work with tingling throughout the body to replace the pain. With new devices, largely the patients don’t have to feel anything; the pain just goes away. The devices also had to be recharged frequently; [newer] devices don’t have to be recharged ever, so the patient gets an implant—you don’t feeling tingling with it, the pain goes away, and the battery lasts about five years.
These therapies will be increasingly available to patients who would have been previously placed on chronic opioid medicines.