Data analytics firms across many different markets are providing solutions to help companies extract value from data. Artificial intelligence (AI) applied to healthcare includes a collection of technologies that enable machines to sense, interpret, act and learn. With the evolution of data analytics—whether applied to big data, population health, practice-specific data or patient-specific data—healthcare services are exponentially expanding their ability to leverage artificial intelligence for use cases such as diagnostics, personalized treatment, imaging analysis, patient trend analysis, outcomes predictions, automation and more.
The addition of IoT sensor data from connected health and related devices adds a new layer of critical, real-time data. These use cases exemplify how artificial intelligence and machine learning can further transform healthcare functions into data-driven services that can improve outcomes and deliver healthcare more efficiently.
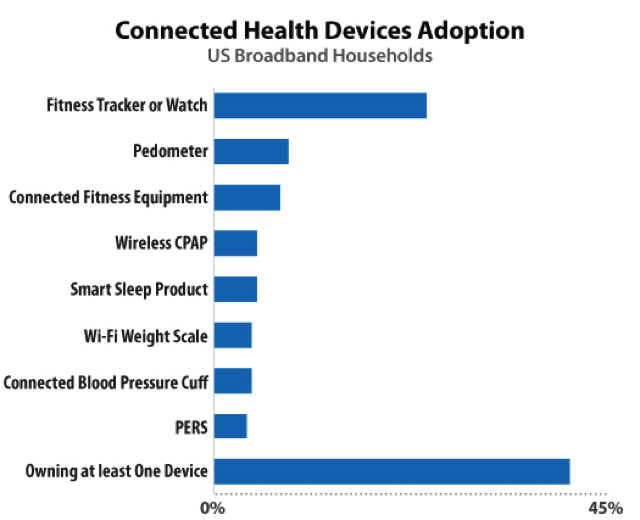
Consumer ownership of health IoT products has risen dramatically in the past few years, driven by booming wearables adoption and consumer health concerns during the COVID-19 pandemic. Connected health device ownership has increased to where 46% of U.S. broadband households own at least one product and 19% own at least two (see Figure 1). AI is figuring prominently in the apps that support these devices whether it is used for applying machine learning to behavioral activity and personal health data, for supporting voice and text bot interactions, or for delivering more personalized and predictive services.
Remote Patient Management and Virtual Care
Remote patient management (RPM) may be applied to a variety of patient populations including those recently discharged after surgery, those with chronic diseases, aging adults and other vulnerable populations. More recently, RPM has been used to monitor COVID-19 patients outside of the clinic, analyzing trends and altering patients and providers if the patient required further assistance. The primary goal of RPM is to provide insight into the ongoing health status of the patient outside of clinical contexts. AI and ML are applied to the data in order to identify the need for interventions that could head off a readmission, address declines before the patient’s condition worsen, or to support better daily management of diseases.
RPM is most valuable for patients with one or more chronic conditions such as congestive heart failure, chronic obstructive pulmonary disease, coronary artery disease, diabetes, hypertension, and asthma. Though RPM solutions may sometimes cross over into independent living solutions for seniors and their family caregivers, they typically involve connecting the at-home patient with their care team, and sometimes insurers. The emphasis of RPM is more on monitoring for the purpose of healthcare and health outcomes than on monitoring for safety, security or comfort.
RPM technology may record a patient’s vital signs, activities of daily living, dietary habits, medications compliance and more. Solutions may be condition-specific, or may be intended for more complex multi-condition treatment. Machine learning algorithms can trigger alerts and notifications resulting in rapid interventions, significantly improved communications, better patient care, and better outcomes at lower costs than traditional healthcare delivery. Machine learning applications also are used to train monitoring systems on massive data sets, perform predictive modeling of illness progression and support behavioral change.
Independent Living and Aging in Place
As of 2019, according to the U.S. Census Bureau, some 53 million Americans were over the age of 65. The vast majority of them (84%) find it very important (rating 6–7 on a 7-point scale) to live independently in their own home as long as possible. The physical and cognitive effects of aging and chronic medical conditions present challenges for those desiring to live independently as well as for their caregivers who worry about keeping them safe, comfortable and socially connected. With the aging demographics of the U.S. population enlarging the senior market, a growing number of companies are offering assistive technology that can improve seniors’ safety and wellness in their own homes, and enhance communication with loved ones. Many of these solutions are applying various AI applications to empower and care for aging adults.
Chronic Disease Management
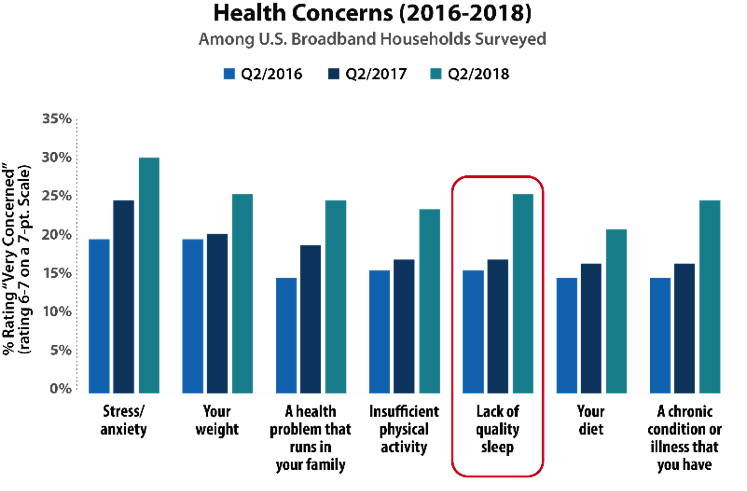
The proliferation of smartphones and connected medical devices is providing new opportunities for helping those living with chronic conditions to monitor and manage them for improved health and safety. Nearly two-thirds of consumers in U.S. broadband households report at least one tested chronic condition and 36% have two or more. Robust solutions are coming to market for supporting patients with diabetes, heart disease, obesity and sleep disorders. As with other AI applications, machine learning is first trained on large data sets of specific populations to identify patterns of disease progression and behavioral patterns that drive changes in health status. Data from personal medical devices, smart sensors, electronic health records, and behavioral activities such as diet, exercise and stress levels can be fused to uncover insights into why health status may change. Prediction and recommendation engines can inform behavioral change engagements through apps and other interfaces.
Challenges and Evolution
AI implementations for digital health can be relatively simple when they are focused largely on patient engagement or vastly complex when working with big data sets, highly specialized diagnostics and the workflows of multiple complex organizations. Still, where there’s an incentive, there’s a way, and financial incentives for healthcare AI are driving unprecedented investment in the technologies. In 2018, CMS introduced current procedural terminology (CPT) codes for delivering RPM services to patients. Over the past several years these have evolved to align with remote patient monitoring best practices, and providers are now being compensated more fairly for all the tasks involved in delivering remote monitoring. This alignment of incentives along with a growing track record of efficacy, savings, and patient satisfaction is expected to drive substantial growth in RPM in the coming years. Healthcare access shortages are also driving RPM as over 136 rural hospitals have close since 2010—and 20 of those hospitals in in the past year alone, as per the Cecil G. Sheps Center for Health Services Research.
The business model for independent living and aging-in-place solutions still largely follows the private pay subscription model but both seniors and their caregivers indicate a strong interest in paying for these services. Recent survey data notes 73% of family caregivers report interest in at least one tested solution aimed at helping their loved one live independently. Further, almost half of these family caregivers are willing to pay $40/month for a professional monitoring service incorporated into their solution of choice. New B2B opportunities are emerging for independent living solutions customized for senior living facilities and communities.
Finally, the high cost of managing chronic conditions is driving healthcare companies to invest and innovate using AI technologies. Strong ecosystems are developing among sensor and device makers, platform providers, data science software developers, user experience experts and behavioral scientists, providers, and payers. Behavioral change is a difficult and complex task but the personalized experiences enabled by AI technologies offer promising new tools for engaging patients every day of their lives.