CMS has three criteria for evaluating whether a technology qualifies for the new technology add-on payment (NTAP) program. This column presents information on which of the three criteria has been the biggest stumbling block for applicants. The answer may surprise you.
What is an NTAP?
The Centers for Medicare and Medicaid Services (CMS) established the NTAP to provide additional payment to hospitals for costs associated with new medical technology that would not otherwise be reflected in Medicare inpatient payment upon initial introduction of the technology. Because CMS uses past claims data to recalibrate the Medicare Severity Diagnosis Related Group (MS-DRG) system, new technologies are not reflected in those past claims and therefore, payment to hospitals may not reflect the new technology costs they incur in a given year.
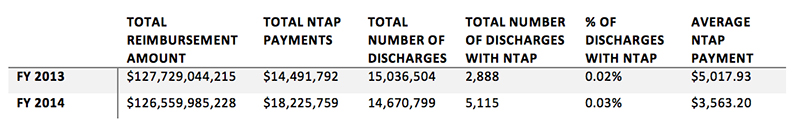
Recent data give us some insight into how NTAP payments impact inpatient payment as a whole. NTAP is only applied to 0.02–0.03% of the number of discharge claims submitted to Medicare contractors for payment.1
In the 12+ years since the implementation of NTAP, CMS has documented in the public domain through final rulemaking published in the Federal Register their decisions and rationale for every application submitted.2 Through this documentation, we are able to learn about how CMS makes their decisions.
NTAP Eligibility Criteria
CMS evaluates NTAP applications based on three criteria in every Federal fiscal year (FY) cycle: Newness, substantial clinical improvement, and cost. Figure 1 shows the relative success applicants have had since the inception of NTAP. On average, for every one approved application since FY 2003, two are either withdrawn midway through the process or denied in final rulemaking after public comment.t
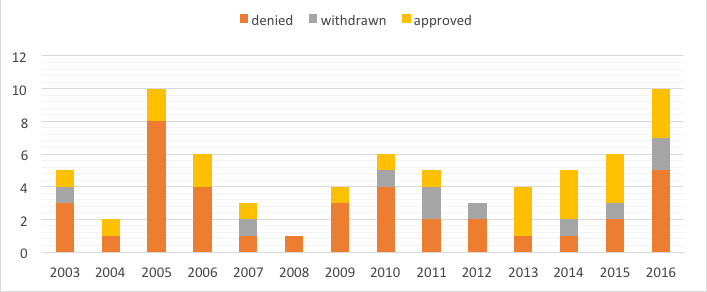
Rather than focusing on the “winners,” let’s review what we can learn from those who have not been able to secure an NTAP.
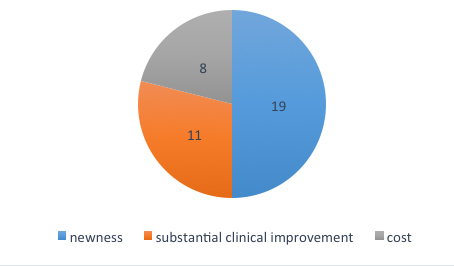
While a considerable portion of the application is dedicated to establishing that a new technology meets the substantial clinical improvement criterion, or meets cost thresholds for demonstrating that the technology otherwise would not be adequately paid under the current DRG framework, we find that the majority of NTAP application denials were a result of not meeting CMS’ newness criterion. Newness is defined as the first commercial distribution of the technology being sufficiently recent so that cost of the technology is not reflected in the data used to calculate DRG relative weights.
So why is newness, the NTAP criterion that appears to be relatively straightforward to meet compared to the other two criteria, so difficult to establish? CMS clarifies that a medical service or technology may be considered new within two to three years after claims data become available reflecting the procedure code assigned to the new service or technology. CMS states, “After CMS has recalibrated the DRGs based on available data that reflects the costs of an otherwise new medical service or technology, the medical service or technology will no longer be considered ‘new’ under this criterion.”3 Let’s review a couple of recent NTAP denials to see if we can glean some insight into how CMS determines newness.
VERASENSE Knee Balancer System (VKS) for FY 2016 (OrthoSensor): How CMS Uses Substantial Similarity in Assessing Newness
VERASENSE is a sensor assisted surgery technology that provides intraoperative feedback to dynamically balance the patient’s knee during total knee arthroplasty (TKA) surgery. VERASENSE was initially approved by the FDA in 2009 but was not made commercially available in the United States until late 2011. Product redesigns and advancements led to additional FDA clearances in 2013. The FY 2016 applicant, OrthoSensor, maintained that VERASENSE met the newness criterion for FY 2016 because the most current version of the product was first commercially available within the two- to three-year eligibility timeframe if using the last FDA clearance date in 2013.
CMS applied a set of “substantially similar” criteria to evaluate whether the 2013 version of the product was different enough from the 2011 version to justify using the 2013 FDA clearance date as the date of first commercial availability. CMS’ assessment was that (a) the two products had the same mechanism of action, (b) cases involving the first version of the product would be assigned to the same MS-DRG as the second version of the product, and (c) both product versions would treat the same diseases and patient populations. Because of this, CMS determined that the 2011 and 2013 versions of VERASENSE were “substantially similar” and therefore did not meet the newness criterion under NTAP. (Incidentally, another FY 2016 applicant’s technology, Astellas Inc.’s CRESEMBA, did not meet the newness criterion based on a similar assessment of substantial similarity to other existing antifungal drugs currently available to Medicare beneficiaries.)
Heli-FX EndoAnchor System (Aptus Endosystems, Inc.): How CMS Anchors Newness to a Six Month Window
The Heli-FX EndoAnchor System is a mechanical fastening device that is designed to enhance the long-term durability and reduce the risk of repeat interventions in endovascular aneurysm repair (EVAR) and thoracic endovascular aneurysm repair (TEVAR). The FY 2015 applicant, Aptus Endosystems, Inc., indicated that the product was cleared by the FDA in 2011. Only four implantations for Medicare beneficiaries occurred between November 2011 and June 2012.
CMS states, “We have generally followed a guideline that uses a six-month window, before and after the beginning of the fiscal year, to determine whether to still consider a technology ‘new’ and extend approved new technology add-on payments for an additional fiscal year. In general, a technology is still considered ‘new’ (and eligible to receive new technology add-on payments) only if the three-year anniversary date of the product’s entry on the market occurs in the latter half of the fiscal year.”4 Based on this benchmark, CMS determined Heli-FX EndoAnchor System did not meet the newness criterion. CMS indicated that these four procedures were already reflected in the Medicare claims data, allowing these procedure costs to influence recalibration of the MS-DRG relative weights, and therefore, payment.
Conclusion
Perhaps surprisingly, of the three eligibility criteria for CMS’ NTAP, the newness criterion has been the most common reason cited by CMS for application denials. CMS may not evaluate the substantial clinical improvement and cost criteria without applicants first meeting the newness criterion. We see through published rule making that applicants must review NTAP history in order to better understand the nuances of meeting the newness criterion for a successful NTAP.
References
- Medicare Provider Analysis and Review (MEDPAR) File, FY 2013 and FY 2014 are the only years to date that NTAP data is available in full.
- Except those applications withdrawn prior to CMS decision.
- 42 CFR Part 412
- 42 CFR Parts 405, 412, 413, 415, 422, 424, 485, and 488




